I plan to do the Cushing's Awareness Challenge again. Last year's info is here: https://cushieblogger.com/2017/03/08/time-to-sign-up-for-the-cushings-awareness-challenge-2017/
This original page is getting very slow loading, so I've moved my own posts to this newer blog.
As always, anyone who wants to join me can share their blog URL with me and I'll add it to the links on the right side, so whenever a new post comes up, it will show up automatically.
If the blogs are on WordPress, I try to reblog them all to get even more exposure on the blog, on Twitter and on Facebook at Cushings Help Organization, Inc. If you have photos, and you give me
permission, I'll add them to the Pinterest page for Cushing's Help.
The Cushing’s Awareness Challenge is almost upon us again!
Do you blog? Want to get started?
Since April 8 is Cushing’s Awareness Day, several people got their heads together to create the Eighth Annual Cushing’s Awareness Blogging Challenge.
All you have to do is blog about something Cushing’s related for the 30 days of April.
There will also be a logo for your blog to show you’ve participated.
Please let me know the URL to your blog in the comments area of this post, on the Facebook page, in one of the Cushing's Help Facebook Groups, on the message boards or an email and I will list it on CushieBloggers ( http://cushie-blogger.blogspot.com/ )
The more people who participate, the more the word will get out about Cushing’s.
Suggested topics – or add your own!
- In what ways have Cushing’s made you a better person?
- What have you learned about the medical community since you have become sick?
- If you had one chance to speak to an endocrinologist association meeting, what would you tell them about Cushing’s patients?
- What would you tell the friends and family of another Cushing’s patient in order to garner more emotional support for your friend? challenge with Cushing’s? How have you overcome challenges? Stuff like that.
- I have Cushing’s Disease….(personal synopsis)
- How I found out I have Cushing’s
- What is Cushing’s Disease/Syndrome? (Personal variation, i.e. adrenal or pituitary or ectopic, etc.)
- My challenges with Cushing’s
- Overcoming challenges with Cushing’s (could include any challenges)
- If I could speak to an endocrinologist organization, I would tell them….
- What would I tell others trying to be diagnosed?
- What would I tell families of those who are sick with Cushing’s?
- Treatments I’ve gone through to try to be cured/treatments I may have to go through to be cured.
- What will happen if I’m not cured?
- I write about my health because…
- 10 Things I Couldn’t Live Without.
- My Dream Day.
- What I learned the hard way
- Miracle Cure. (Write a news-style article on a miracle cure. What’s the cure? How do you get the cure? Be sure to include a disclaimer)
- Give yourself, your condition, or your health focus a mascot. Is it a real person? Fictional? Mythical being? Describe them. Bonus points if you provide a visual!
- 5 Challenges & 5 Small Victories.
- The First Time I…
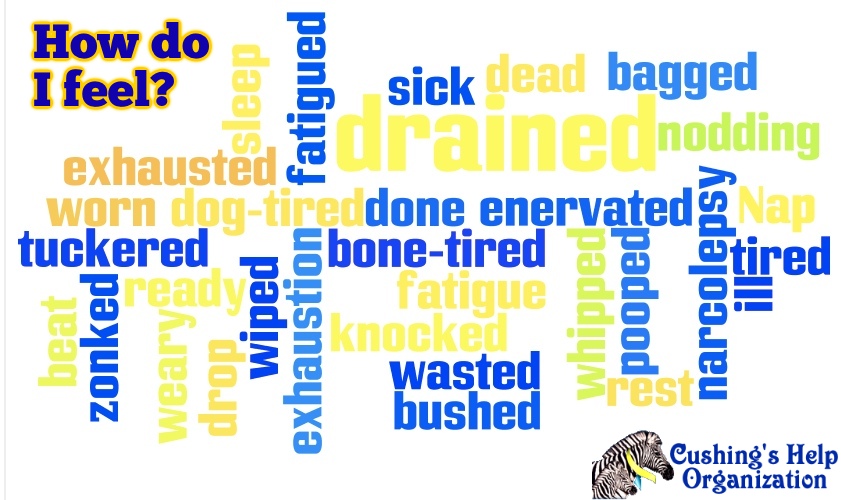
- Make a word cloud or tree with a list of words that come to mind when you think about your blog, health, or interests. Use a thesaurus to make it branch more.
- How much money have you spent on Cushing’s, or, How did Cushing’s impact your life financially?
- Why do you think Cushing’s may not be as rare as doctors believe?
- What is your theory about what causes Cushing’s?
- How has Cushing’s altered the trajectory of your life? What would you have done? Who would you have been
- What three things has Cushing’s stolen from you? What do you miss the most? What can you do in your Cushing’s life to still achieve any of those goals?
- What new goals did Cushing’s bring to you?
- How do you cope?
- What do you do to improve your quality of life as you fight Cushing’s?
- How Cushing’s affects children and their families
- Your thoughts…?